Healthcare Fraud Investigations – What Does the Government Look For?
Federal and state prosecutors are increasingly aggressive in their investigation and prosecution of healthcare fraud. Given the vast amounts of government or private insurance monies that can be exploited, the penalties have increased for healthcare professionals and others who engage in fraudulent activities. Sentences of 10 years or more, in addition to forfeitures, restitution and fines in the millions of dollars, are becoming commonplace.
So, what do investigators look for when investigating fraud? They examine what has become known as the “badges of fraud”, meaning the red flags that investigators target.
First, healthcare fraud referrals often come from insurance companies who have noticed discrepancies in a provider’s billing practices. These could include:
- An unusually high number of procedures compared with similar practitioners
- Indicia of “upcoding” – billing a simple procedure at a code for a more time consuming, complex procedure that results in greater reimbursement by the insurer
- Submitting a large number of bills all at once shortly before the period for reimbursement expires
- An excessive number of patient visits in a given time period, or
- An unusually high number of out-of-network procedures
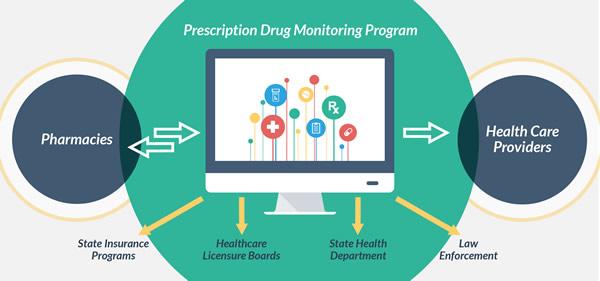
Second, investigators key in on certain types of practices that historically are ripe for abuse. Any practitioner who prescribes opioids will receive heightened scrutiny. The physician’s practice, the number of repeat patients for opioids, the geographic areas the patients are coming from, the amount of prescriptions, and the histories of the patients all provide avenues of investigation and potential red flags. In addition, Prescription Drug Monitoring Programs alert authorities to patients that fill prescriptions for certain drugs from multiple physicians.
Third, the government has recently charged scores of doctors and individuals involved in compounded medicines, such as pain cremes, vitamins and scar creams. The medications, which the government deems medically unnecessary, are extremely expensive, often costing thousands of dollars for a tube of ointment. The patient population targeted by marketers was simply based on whether their insurance reimbursed for these medications, rather than a true medical need for the compounded medicine.
Fourth, investigators examine certain types of practices that use unqualified or unlicensed workers that are billed at qualified professional rates for procedures or require supervision by medical professionals who are not present for the treatments. The insurers are defrauded when these practices submit bills for procedures that are supposed to be preformed or supervised by licensed healthcare professionals at a higher rate, but are actually performed by others to increase the volume of insured procedures.
Experienced Defense Halthcare Fraud Attorneys
For questions regarding health care, Medicaid or Medicare fraud, contact Stahl Gasiorowski Criminal Defense Lawyers. Our offices are located in Mountainside, New Jersey, and New York City. Contact us online or call us at 908-301-9001.
Our goal is to prevent you from being charged once an investigation begins. If you are the target of an investigation, we can work effectively with the goal of averting charges, reducing charges or winning full acquittal in court.